Contents
Exploring Nerve stimulation
Nerve stimulation, a cutting-edge technique in modern medicine, is crucial in pain management and neurological rehabilitation. This method involves applying electrical impulses to specific nerves and altering their activity to achieve therapeutic outcomes. Various types of nerve stimulation include Transcutaneous Electrical Nerve Stimulation (TENS), which doctors commonly use for pain relief, and Spinal Cord Stimulation (SCS), which helps manage chronic pain conditions. Deep Brain Stimulation (DBS), targets neurological disorders such as Parkinson’s disease and essential tremors. Additionally, Vagus Nerve Stimulation (VNS) is employed to treat epilepsy and depression. Thus, each of these techniques offers unique benefits, providing relief and improved quality of life for patients with different medical conditions
Transcutaneous Electrical Nerve Stimulation (TENS)
Transcutaneous Electrical Nerve Stimulation (TENS) utilizes low-voltage electrical pulses to reduce chronic and acute pain. This therapy works by sending electrical impulses through electrodes placed on the skin, targeting specific nerve pathways to disrupt pain signals before they reach the brain. This therapy will stimulate the endorphins, the natural pain relief hormone. The electrodes are attached to either side of the pain area at a distance of at least 2.5 cm apart. When the electrical impulses flow through the painful area it may feel a tingling sensation
TENS is widely used for various conditions, including arthritis, back pain, sports injuries, and postoperative discomfort. It provides drug-free pain management, reducing reliance on medication and minimizing potential side effects. It is Easy to use and portable, TENS devices are ideal for home use, allowing individuals to manage their pain conveniently and effectively. Thus, TENS therapy can lead to improvements in pain control without the use of medications.
Understanding the Different Types of TENS Units for Pain Relief
Conventional TENS
Conventional Transcutaneous Electrical Nerve Stimulation (TENS) is a widely used method for managing chronic and acute pain. This approach employs high-frequency, low-intensity electrical currents delivered through electrodes placed on the skin, which effectively block pain signals from reaching the brain. Conventional TENS is beneficial for treating conditions such as arthritis, back pain, and muscle strain. So, this makes people’s lives easier without relying on medications.
Acupuncture- Like TENS
This technique involves delivering low-frequency, high-intensity electrical pulses to mimic the effects of acupuncture needles, stimulating specific points in the body to alleviate pain. Acupuncture- like TENS is particularly effective for treating deep, chronic pain conditions such as fibromyalgia, sciatica, and chronic back pain. By promoting the release of endorphins and improving blood flow, this method offers a natural and holistic approach to pain management.
Intense TENS
Intense Transcutaneous Electrical Nerve Stimulation (TENS) is designed for individuals who require robust pain relief due to severe or persistent pain conditions. This method utilizes high-frequency, high-intensity electrical currents to deliver powerful pain-blocking signals through the skin to the affected nerves. Doctors often recommend intense TENS for acute pain episodes, postoperative pain, and severe musculoskeletal injuries. So, its potent stimulation can quickly reduce pain intensity, providing fast and effective relief.
TENS Therapy Safe? Potential Side Effects
While Transcutaneous Electrical Nerve Stimulation (TENS) is generally a safe treatment with no significant side effects, there are some considerations to be aware of. Certain individuals may experience skin irritation or redness due to an allergic reaction to the adhesive pads. Doctors do not recommend TENS for individuals with pacemakers or other electrical or metal implants. Pregnant women, particularly in the early stages of pregnancy, should avoid TENS unless advised otherwise by their healthcare provider. Those with epilepsy, heart problems, or an overactive bladder should also exercise caution and consult with their doctor before using TENS therapy.
Vagus Nerve Stimulation (VNS)
Vagus Nerve Stimulation (VNS) therapy is a treatment for individuals suffering from epilepsy and treatment-resistant depression. This involves implanting a small device under the skin, which sends mild electrical pulses to the vagus nerve in the neck and this therapy is approved by the Food and Drug Administration (FDA). These pulses help regulate brain activity, reducing the frequency and intensity of seizures and improving mood. VNS therapy is particularly beneficial for patients who have not responded well to traditional medications. Thus, it may assist in elevating your mood and easing depressive symptoms.
Vagus Nerve Stimulation: A Breakthrough in Stroke Recovery
The FDA-approved vagus nerve stimulation (VNS) device is now being utilized in stroke rehabilitation to aid recovery. When a person experiences difficulty using their hand or arm following a stroke, the VNS device delivers mild electrical stimulation to the vagus nerve. This stimulation, combined with targeted exercises, promotes the formation of new neural pathways in the brain, enhancing the person’s ability to regain function and improve motor skills.
The device sends electrical impulses along the left vagus nerve to the brainstem. The device will be connected with wires to the vagus nerve on the left side of your neck, a nerve that naturally transmits signals to the brain. The right vagus nerve is generally avoided in this therapy, as its stimulation could impact heart function. Thus, VNS device produce electrical impulses to stimulate the vagus nerve, delivering these impulses for 30 seconds every 5 minutes.
Treating Headaches and Migraines with Non-Invasive Vagus Nerve Stimulation
Non-invasive vagus nerve stimulation devices, which do not require surgery, have been approved by the FDA for treating cluster headaches and migraines in the United States. These devices work by stimulating the vagus nerve when held against the skin of the neck. So, this stimulation helps block pain signals, effectively preventing or alleviating head pain.
Peripheral Nerve Stimulation (PNS)
A chronic discomfort was treated by peripheral nerve stimulation. Doctors implant a wire-like electrode adjacent to the peripheral nerve. These are the nerves that reach beyond the spinal cord and brain. Patients feel quick electrical pulses from the electrode as light tingles. Doctors conduct a trial before implantation, connecting the electrodes to an external device. When the trial is successful, the patient will have an implant with a tiny generator.
Patients who have localized nerve pain include;
- secondary to trauma,
- prior surgery,
- amputation, or even diabetes.
This therapy is used for patients with complex regional pain syndrome (CRPS). Without the proper knowledge of location of the nerve, it may leads to destruction of blood vessels. Doctors use ultrasound to place the peripheral nerve, which helps reduce the risk. Thus, ultrasound-guided placement of electrodes will help implant properly at the nerves.
Spinal Nerve Stimulation (SNS)
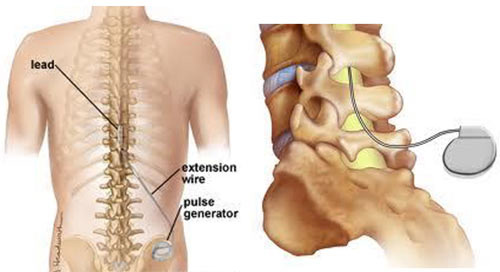
An implanted device known as a spinal cord stimulator delivers low levels of electricity directly into the vertebral column in order to decrease discomfort. Spinal cord stimulators consist of thin wires called electrodes and a small battery pack. Doctors place the electrodes between the vertebrae and the spinal cord (in the epidural space), and they position the generator under the skin, typically near the buttocks or abdomen. Patients can trigger the electrical impulses with a remote control when they experience pain.
A flexible therapy that can greatly improve quality of life and sleep patterns while lowering the need for painkillers is spinal cord stimulation. It is very useful in treating a variety of pain conditions, such as chronic back pain following surgery, arachnoiditis, spinal cord injuries, and pain connected to nerves, such as severe diabetic neuropathy and pain related to cancer from radiation, surgery, or chemotherapy. Doctors can use this therapy to treat visceral abdominal pain, post-amputation pain, peripheral vascular disease, and complex regional pain syndrome.
Types of Spinal Nerve Stimulation for Chronic Pain Relief
Conventional Implantable Pulse Generator (IPG)
The Conventional Implantable Pulse Generator (IPG) is a type of spinal cord stimulator that uses a battery-powered device implanted under the skin, typically in the lower back or abdomen. This device delivers electrical pulses to the spinal cord, which helps to mask pain signals before they reach the brain. It should be replaced between 2 to 5 years.
Rechargeable Implantable Pulse Generator (IPG)
The Rechargeable Implantable Pulse Generator (IPG) offers a long-lasting solution for spinal cord stimulation with the convenience of a rechargeable battery. Doctors insert it beneath the skin to reduce pain by electrically stimulating the spinal cord. Thus, it reduces the need for frequent surgical replacements. So, this therapy can treat Long-term pain management.
Radiofrequency Stimulator
The Radiofrequency Stimulator uses radio waves to power the device, eliminating the need for an internal battery. An external transmitter sends radiofrequency waves to the implanted receiver, which then generates electrical impulses. This allows for unlimited usage without the concern of battery depletion. This provides high-power stimulation and allows for easy adjustment to meet individual pain management needs.
Deep Brain Stimulation (DBS)
Individuals with mobility disorders can be treated with deep brain stimulation. These disorders include dystonia, Parkinson’s disease, and essential tremor. Doctors also treat psychiatric disorders, including obsessive-compulsive disorder, with Deep Brain Stimulation. The Food and Drug Administration has approved Deep Brain Stimulation as a therapy for seizures. When medication cannot control a patient’s symptoms, doctors perform deep brain stimulation.
Deep brain stimulation (DBS) involves creating small holes in the skull to implant electrodes into the brain tissue. Surgical complications may include the misplacement of the electrode leads, brain bleeding, stroke, infection, breathing difficulties, nausea, heart issues, and seizures. Post-surgery side effects can include seizures, infections, headaches, confusion, difficulty concentrating, strokes, and hardware complications such as eroded lead wires. Patients may also experience temporary pain and swelling at the implantation site.
Procedure
A special head frame keeps the patient’s head still. Doctors use a brain MRI or CT scan to map the brain and accurately place the electrode. They then insert the lead into a specific area of the brain. A surgeon places the pulse generator under the skin near the collarbone. The person can operate the pulse generator externally, adjusting the impulses according to their condition. Thus, using a remote control, they can turn the stimulation on or off as needed.
Occipital Nerve Stimulation (ONS)
Occipital nerve stimulation (ONS) actively treats chronic headaches and certain types of neuropathic pain through a medical procedure. It involves the implantation of a small device that sends electrical impulses to the occipital nerves located at the base of the skull. These nerves are responsible for transmitting sensory information from the scalp to the brain. By delivering targeted electrical stimulation, ONS can modulate pain signals and provide significant relief to patients suffering from conditions such as occipital neuralgia, migraines, and cluster headaches.
Conclusion
In conclusion, various nerve stimulation techniques, including Transcutaneous Electrical Nerve Stimulation (TENS), Peripheral Nerve Stimulation (PNS), Vagus Nerve Stimulation (VNS), Deep Brain Stimulation (DBS), and Occipital Nerve Stimulation (ONS), represent advancements in the reducing chronic pain and neurological disorders. Each technique offers unique benefits tailored to specific conditions: TENS provides non-invasive pain relief through surface electrodes; PNS targets specific peripheral nerves to alleviate localized pain; VNS modulates brain activity through the vagus nerve, benefiting epilepsy and depression patients; DBS involves implanting electrodes in the brain to treat movement disorders like Parkinson’s disease; and ONS focuses on alleviating headaches and neuropathic. These therapies enhance patient outcomes by offering personalized and effective treatment.
Source
- https://www.nhs.uk/conditions/transcutaneous-electrical-nerve-stimulation-tens/#:~:text=Transcutaneous%20electrical%20nerve%20stimulation%20(TENS,to%20sticky%20pads%20called%20electrodes.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4589923/
- https://www.mayoclinic.org/tests-procedures/vagus-nerve-stimulation/about/pac-20384565
- https://www.mind.org.uk/information-support/drugs-and-treatments/vagus-nerve-stimulation-vns/#:~:text=Some%20people%20can%20feel%20a,the%20benefits%20of%20this%20treatment
- https://www.neuromodulation.com/PNS
- https://health.ucdavis.edu/pain/specialties/Peripheral-Nerve-Stimulation.html
- https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/treating-pain-with-spinal-cord-stimulators
- https://www.mayoclinic.org/tests-procedures/deep-brain-stimulation/about/pac-20384562
- https://www.ncbi.nlm.nih.gov/books/NBK553129/#:~:text=ONS%20is%20a%20minimally%20invasive,distribution%20of%20the%20occipital%20nerve
- https://www.defeatingepilepsy.org/treatment-for-epilepsy/deep-brain-stimulation/
- https://www.healthline.com/health/tens-unit-for-lower-back-pain-placement#placement
Written by Snegkha S

Pingback: Thyroid Hormones and Behavioral Changes